Outpatient Mental Health Discharge Summary Template
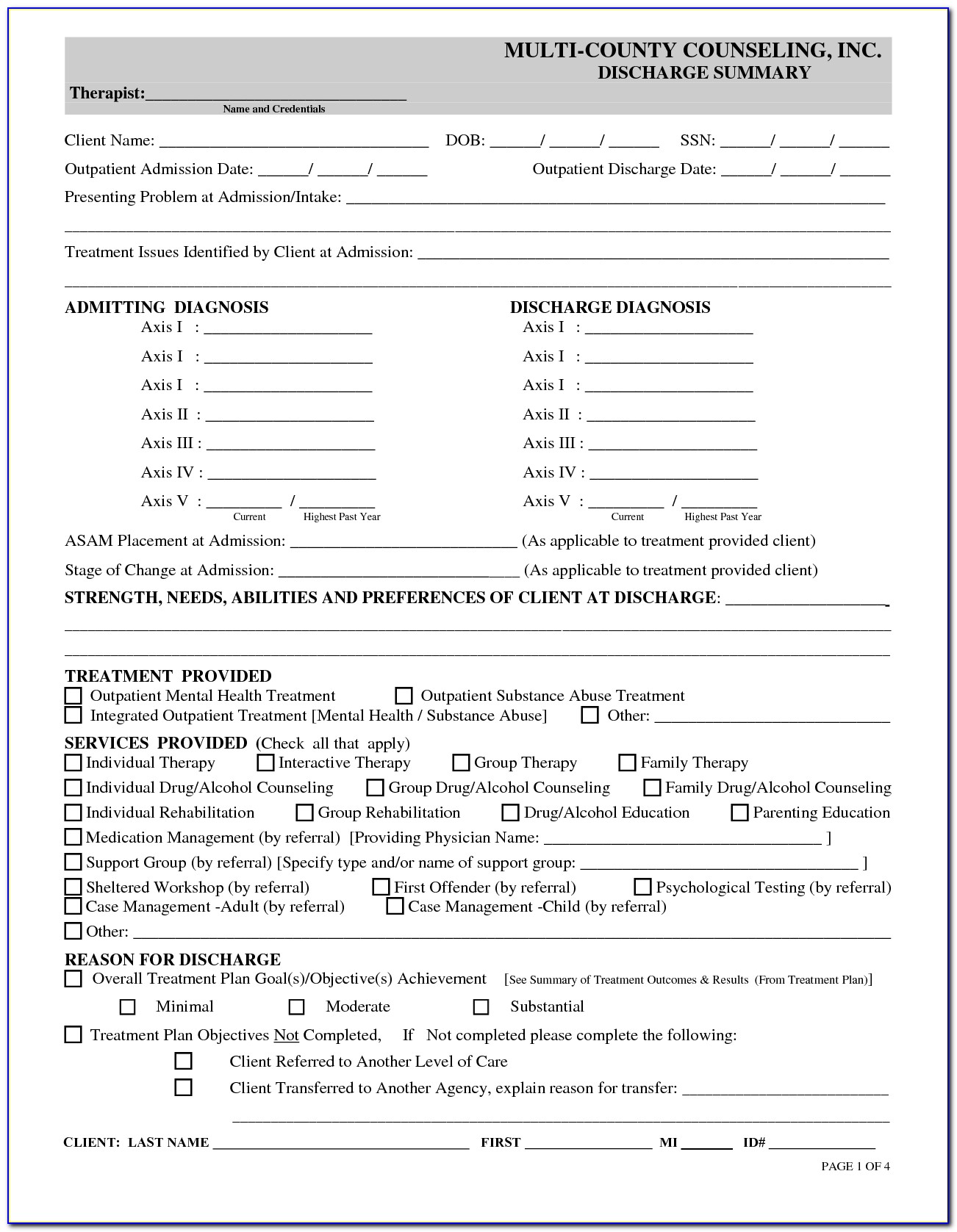
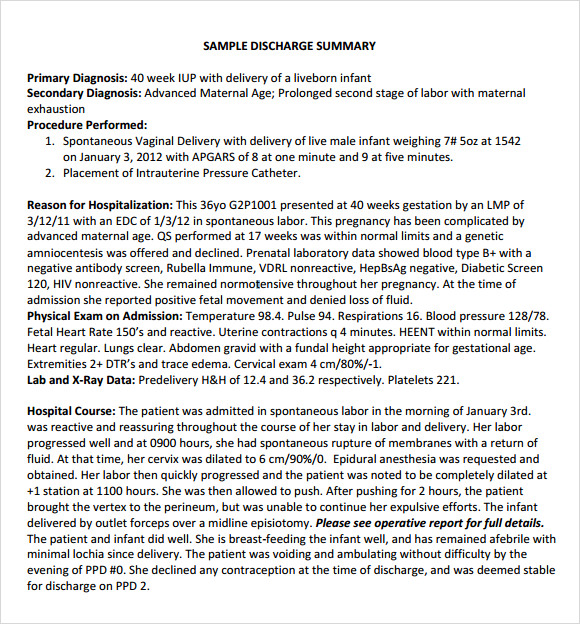
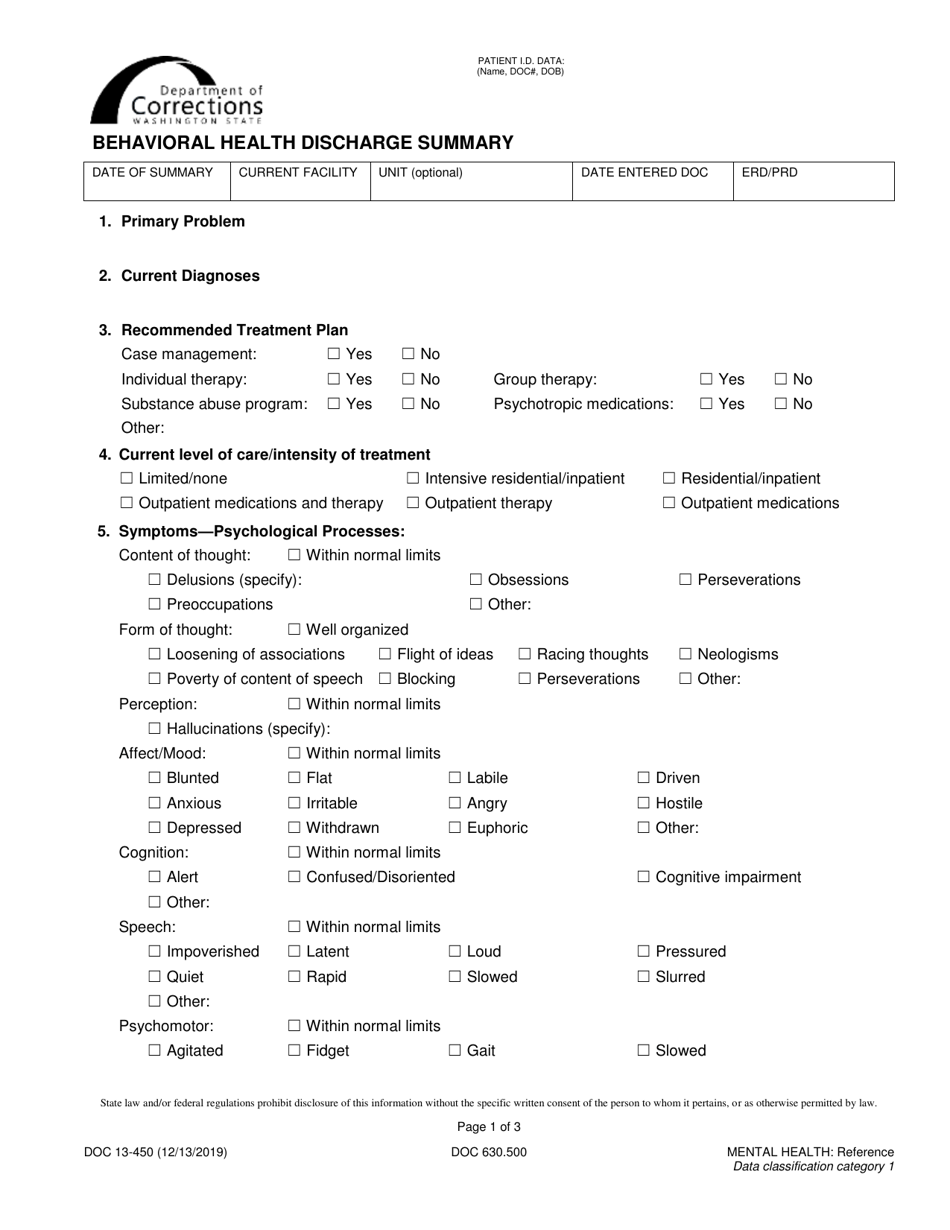
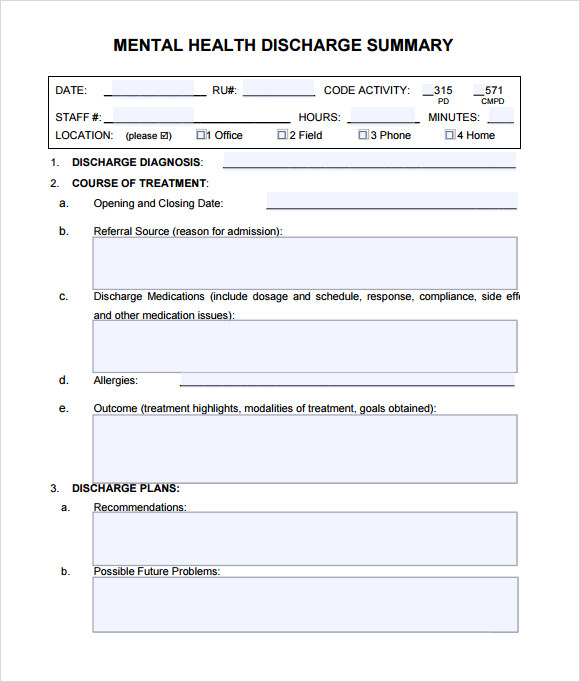
Outpatient Mental Health Discharge Summary Template - A discharge note, also called a termination note, is a written summary held in the client’s chart of what happened during the time the client was in your care. Web behavioral health issues, ed. Cover page with initial psychiatric assessment; Bipolar disorder, depressed, with psychotic features, symptoms in remission. Ad use the only ehr with a fully integrated website builder to help clients find you. Mental health discharge summary/billing form. All progress notes in a compressed format (optional) final page with patient. A progress note typically uses a soapor girpformat and documents weekly sessions. See why therapynotes is the leading ehr software for mental health clinics. Web core functions of a discharge planner may include: Ad you deserve the best ehr software for mental health. Ad use the only ehr with a fully integrated website builder to help clients find you. This form is being used to (check one): Ditch the expensive developer, and customize your own website with simplepractice. Attention deficit hyperactivity disorder, symptoms in remission. 2/15/1965 date admitted:12/14/2014 date discharged:1/1/2015 this discharge summary and plan. All progress notes in a compressed format (optional) final page with patient. Web good discharge planning can help you get well and avoid having to return to the hospital. Web core functions of a discharge planner may include: It’s available 24 hours a day, 7 days a week. Web 3:15 pm patient name:john doe patient id:10050049 date of birth: Web core functions of a discharge planner may include: Discharge from mhc services transfer to another program. Mental health discharge summary/billing form. Try ours for 30 days free. It’s available 24 hours a day, 7 days a week. Web good discharge planning can help you get well and avoid having to return to the hospital. Ad use the only ehr with a fully integrated website builder to help clients find you. Ditch the expensive developer, and customize your own website with simplepractice. Ad use the only ehr with. A progress note typically uses a soapor girpformat and documents weekly sessions. Malnutrition, weight loss and eating disorders — age > 7 years old,. Ad you deserve the best ehr software for mental health. Try ours for 30 days free. All progress notes in a compressed format (optional) final page with patient. Web our discharge summaries include the following items: Web good discharge planning can help you get well and avoid having to return to the hospital. Suicide risk assessment and care planning, outpatient specialty care. Mental health discharge summary/billing form. Web mental health centerdischarge summary or transition plan. All progress notes in a compressed format (optional) final page with patient. Ditch the expensive developer, and customize your own website with simplepractice. Cover page with initial psychiatric assessment; Ad use the only ehr with a fully integrated website builder to help clients find you. Web our discharge summaries include the following items: Bipolar disorder, depressed, with psychotic features, symptoms in remission. Ad use the only ehr with a fully integrated website builder to help clients find you. A progress note typically uses a soapor girpformat and documents weekly sessions. Mental health discharge summary/billing form. Web behavioral health issues, ed. This veterans health administration (vha) directive describes the procedures and reporting requirements for the mental health residential rehabilitation. Web 3:15 pm patient name:john doe patient id:10050049 date of birth: Attention deficit hyperactivity disorder, symptoms in remission. Cover page with initial psychiatric assessment; Try ours for 30 days free. A progress note typically uses a soapor girpformat and documents weekly sessions. A discharge note, on the other hand, spans a broader amount of. Web core functions of a discharge planner may include: Malnutrition, weight loss and eating disorders — age > 7 years old,. See why therapynotes is the leading ehr software for mental health clinics. Bipolar disorder, depressed, with psychotic features, symptoms in remission. Ad use the only ehr with a fully integrated website builder to help clients find you. Web mental health centerdischarge summary or transition plan. Attention deficit hyperactivity disorder, symptoms in remission. Cover page with initial psychiatric assessment; Discharge from mhc services transfer to another program. 2/15/1965 date admitted:12/14/2014 date discharged:1/1/2015 this discharge summary and plan. A discharge note, also called a termination note, is a written summary held in the client’s chart of what happened during the time the client was in your care. This form is being used to (check one): Web how can i get the discharge summary template? as a resource for sondermind providers, we’ve created a discharge template that you can access here. It’s available 24 hours a day, 7 days a week. Web our discharge summaries include the following items: Nesmith has a history of suicidal thoughts but has never. Ditch the expensive developer, and customize your own website with simplepractice. This veterans health administration (vha) directive describes the procedures and reporting requirements for the mental health residential rehabilitation. Mental health discharge summary/billing form. Web behavioral health issues, ed. Suicide risk assessment and care planning, outpatient specialty care. Ditch the expensive developer, and customize your own website with simplepractice. Ad use the only ehr with a fully integrated website builder to help clients find you. Ditch the expensive developer, and customize your own website with simplepractice. Web mental health centerdischarge summary or transition plan. Bipolar disorder, depressed, with psychotic features, symptoms in remission. All progress notes in a compressed format (optional) final page with patient. Discharge from mhc services transfer to another program. Ad use the only ehr with a fully integrated website builder to help clients find you. Web 3:15 pm patient name:john doe patient id:10050049 date of birth: Web our discharge summaries include the following items: This veterans health administration (vha) directive describes the procedures and reporting requirements for the mental health residential rehabilitation. Nesmith has a history of suicidal thoughts but has never. Suicide risk assessment and care planning, outpatient specialty care. This handout has questions to help you think about your discharge planning and the. A discharge note, on the other hand, spans a broader amount of. Web behavioral health issues, ed. A discharge note, also called a termination note, is a written summary held in the client’s chart of what happened during the time the client was in your care. A progress note typically uses a soapor girpformat and documents weekly sessions.Psychotherapy Discharge Summary Template Jurjur 02A
Pin on social work
Outpatient Mental Health Discharge Summary Template
klauuuudia Discharge Summary Template Mental Health
Patient Discharge Form Download Printable Pdf Templateroller Gambaran
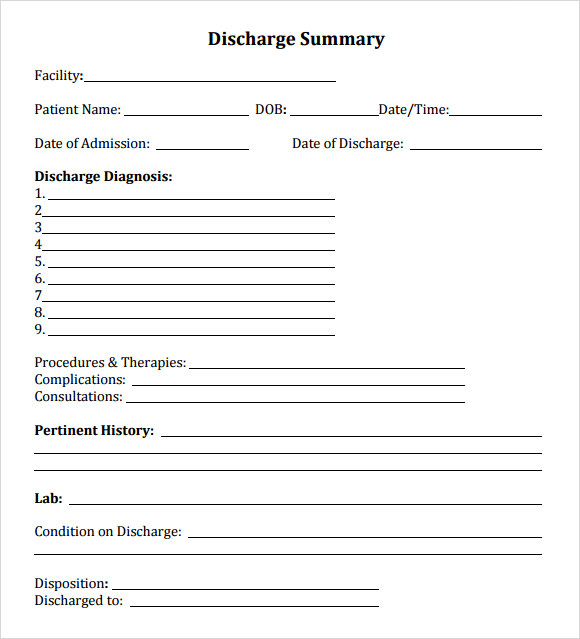
Discharge Summary Template download free documents for PDF, Word and
FREE 7+ Sample Discharge Summary Templates in PDF MS Word
Printable Outpatient Mental Health Discharge Summary Template Excel
8+ Sample Discharge Summary Templates PDF, Word Sample Templates
Discharge Summary Template Mental Health klauuuudia
See Why Therapynotes Is The Leading Ehr Software For Mental Health Clinics.
Web Core Functions Of A Discharge Planner May Include:
Mental Health Discharge Summary/Billing Form.
Ditch The Expensive Developer, And Customize Your Own Website With Simplepractice.
Related Post: